Revolutionizing Respiratory Medicine Through iPSCs and Microfluidics
The urgent need for advanced treatments for respiratory illnesses has led to innovative research methodologies at Kyoto University. With the advent of induced pluripotent stem cells (iPSCs) on microfluidic chips, there is a significant leap in how we can better understand and address complex viral infections such as COVID-19. By modeling distinct lung regions, scientists aim to unravel the underlying pathologies associated with respiratory diseases and deliver personalized healthcare solutions.
The Challenges of Traditional Modeling
Traditional methods for studying respiratory illnesses often involve animal models or in vitro systems that do not accurately reflect the human body’s responses. The responses of various lung regions to viral infections are nuanced and can differ dramatically. This challenge has frustrated researchers for years, leading to slow progress in developing effective treatments. The microphysiological system (MPS) developed by Kyoto University researchers offers a solution by simulating both the airway and alveoli regions of the human lung. This approach provides a more realistic representation of how respiratory infections operate.
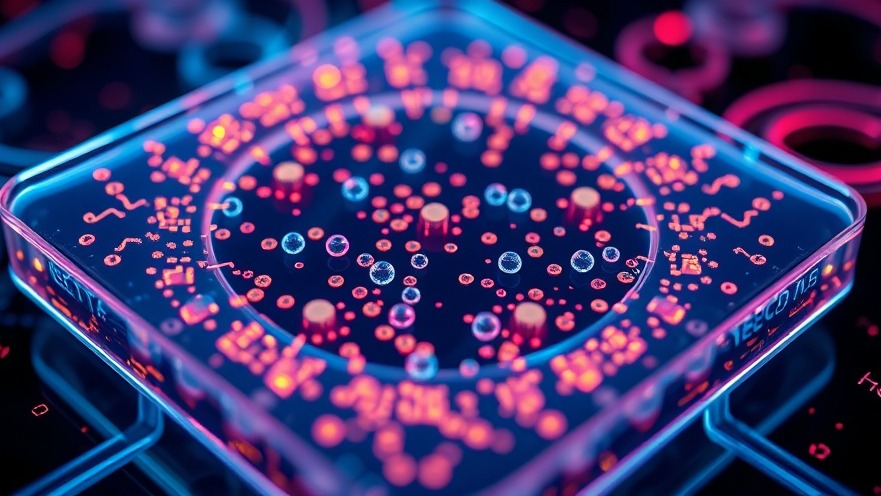
Innovative Design of iPSC-Derived Lung Chips
The introduction of iPSC-derived lung chips allows researchers to model how proximal and distal lung regions respond to different viral pathogens accurately. Using an isogenic source for the iPSCs means that the cells used are genetically identical, which eliminates variability in results and enables more precise observations. The platform’s flexibility makes it suitable for studying a range of lung diseases and could ultimately evolve into a tool for multi-organ studies, enhancing our understanding not just of lung health but of systemic responses to infection.
Future Implications for Pandemic Preparedness
As the world grapples with an increasing number of viral pandemics, this research could have far-reaching implications. Besides offering insights into drug effectiveness and viral pathologies, these tools could facilitate early drug screening, optimizing therapeutic strategies at a more rapid pace. With the capacity to replicate host responses to various viral infections, this research is not only a step forward for personalized medicine but also a proactive approach to future health crises.
Personalized Medicine Through Patient-Specific iPSCs
One of the most exciting components of this research is its potential for personalized medicine. By using patient-specific iPSCs, healthcare practitioners can study an individual's unique lung response to diseases, tailoring treatment plans that are far superior to one-size-fits-all methods. This reinforces the growing trend towards precision medicine in healthcare—an adaptation that could change outcomes for many patients suffering from chronic or acute respiratory conditions.
Actionable Insights for Healthcare Practitioners
For concierge health practitioners and professionals keen on implementing the latest breakthroughs in respiratory medicine, staying informed about emerging technologies such as iPSC-derived lung chips is vital. Understanding these innovations not only enhances patient care but also prepares practitioners for discussions about the future of medical treatments and individual patient management strategies.
Conclusion: The Future of Respiratory Health
The application of iPSCs in microfluidic systems represents a pivotal development in respiratory medicine. As these technologies continue to evolve, the potential they hold for better understanding respiratory diseases and tailoring treatment plans cannot be overstated. Practitioners who embrace this knowledge will be strategically positioned to provide cutting-edge care. For continued advancements in healthcare technology, keeping abreast of research like this is essential for improving patient outcomes.
 Add Row
Add Row  Add
Add 




Write A Comment