Breakthrough in Trauma Care: Bioengineered Blood Vessels Making Waves
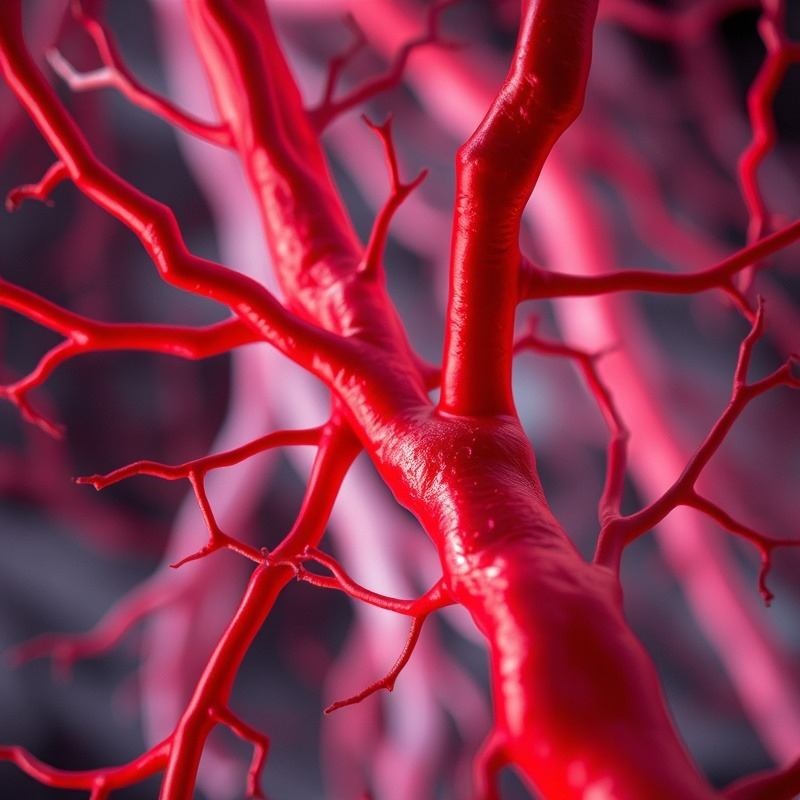
Imagine a world where damage to blood vessels and traumatic injury can be swiftly addressed with new, innovative solutions. Enter bioengineered vessels—an exciting advancement in trauma care that is reshaping how vascular surgery is approached. With a focus on durability and infection resistance, these vessels are offering a promising alternative to traditional methods.
What Are Bioengineered Blood Vessels?
The development of bioengineered blood vessels, also known as acellular tissue-engineered vessels (ATEVs), marks a significant milestone in medical technology. Constructed in the confines of a laboratory, these vessels are grown from cultured human cells which undergo specialized treatment to evade immune rejection when implanted into patients. As time progresses, these vessels invite the patient's own cells to populate, fortifying their resistance to infection—a common pitfall of synthetic grafts. This approach is revolutionizing the treatment of severe vascular injuries.
Field Trials: Promising Outcomes Across Different Settings
In a groundbreaking phase II trial, bioengineered vessels have outperformed traditional synthetic grafts in every measurable way. Conducted across institutions like Rutgers Health, the study amalgamated results from civilian trauma cases in the United States and military casualties in Ukraine. Results from these diverse settings underline their potential impact: 91.5% of these innovative vessels remained functional 30 days post-implantation, compared to only 78.9% with synthetic options. Moreover, the infection rate dropped significantly to less than 1%, a stark contrast to the 8.4% witnessed in synthetic counterparts.
Why This Matters in Urgent Care Scenarios
Trauma surgeons often prefer using a patient's own veins, particularly for critical repairs involving vascular damage. However, factors like the quality of veins and previous surgeries can complicate this preference. Bioengineered vessels not only serve as a highly viable alternative but also expedite the restoration of blood flow—a vital aspect of trauma cases. By reducing the amputation rate from 24.3% to just 4.5%, these vessels don't just save blood flow but preserve livelihoods.
Future Predictions and Trends: The Road Ahead for Bioengineered Solutions
As the FDA has cleared the way for broader use, the stage is set for these bioengineered solutions to potentially join the ranks of standard medical procedures. This technology aligns with trends towards personalized and precision medicine, aiming to reduce reliance on synthetic materials that can carry higher risks of rejection or complication. For medical professionals eager to stay at the cutting edge of patient care, understanding and adopting bioengineered vessels could translate into tangible patient improvements in the immediate future.
Relevance to Current Events: A Global Need
As war and disaster continue to present complex medical challenges worldwide, the application of bioengineered vessels in conflict zones—as seen in the Ukrainian trials—underscores their utility in saving lives under dire circumstances. The global surge in the need for innovative trauma solutions reflects a market adjusting rapidly to these pressing needs, positioning ATEVs as a critical component of future trauma care.
Actionable Insights and Practical Tips
For concierge health practitioners, staying abreast of these advancements can significantly impact patient outcomes. By adopting these bioengineered vessels, practitioners can provide advanced care options especially in urgent cases lacking suitable traditional treatments. Familiarizing oneself with these new methods and discussing their potential with peers can foster a more informed and prepared practice.
 Add Row
Add Row  Add
Add 






Write A Comment