Understanding Uterine and Bladder Prolapse: What You Need to Know
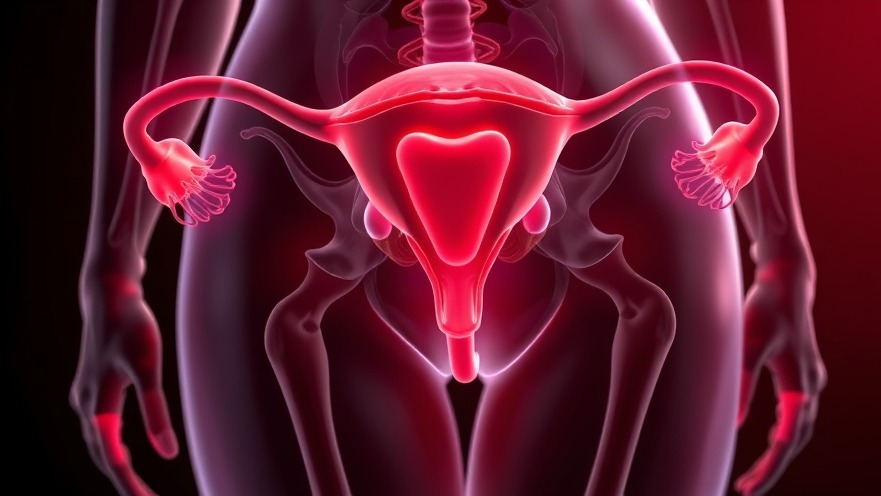
Uterine and bladder prolapse can be an uncomfortable and distressing condition affecting a significant number of women, often going undiagnosed. Essentially, this occurs when the supportive muscles and ligaments in the pelvic region weaken, allowing the organs to sag into the vaginal canal. This can lead to physical discomfort and emotional distress, making it crucial for healthcare providers to be aware of the symptoms and treatment options available.
Symptoms that Matter: Recognizing Prolapse Early
Early detection is key in treating uterine and bladder prolapse effectively. Many women may not experience symptoms in mild cases, but as the condition progresses, it can lead to discomfort in the vagina, pelvis, and lower back. Patients commonly report a sensation of heaviness or pressure, sometimes feeling as though something is falling out of their vagina. These symptoms can worsen during activities such as sexual intercourse and menstruation, further impacting a woman's quality of life.
The Impact of Childbirth and Menopause
Significantly, childbirth is a leading factor in the development of prolapse, especially for women who have multiple pregnancies with vaginal deliveries. The strain on pelvic muscles intensifies over time. Furthermore, hormonal changes during menopause can lead to decreased estrogen levels, which in turn affect the strength of pelvic tissues. For concierge medical practice owners, understanding these connections between reproductive health and pelvic support is vital for offering comprehensive care.
Creating Awareness: The Importance of Patient Engagement
One of the most alarming statistics is that only 10% to 20% of women experiencing symptoms seek medical help. Educating patients about uterine and bladder prolapse should be a priority for medical practices focused on women's health. Concierge practices, in particular, can foster an environment of trust where patients feel comfortable discussing sensitive issues. By promoting a culture of open communication, medical practitioners can enhance patient relationships and encourage proactive health management.
Holistic Care Strategies: Supporting Pelvic Health
Implementing wellness strategies that target pelvic health can be beneficial. This might involve educational workshops, nutritional counseling focused on maintaining a healthy weight, and discussions around lifestyle factors that can alleviate risks associated with prolapse, such as proper posture and strength training. Establishing a solid foundation in wellness not only enhances patient relationships but can also set your practice apart.
A Call to Action: Follow-up Matters
As a concierge medical practice owner, it’s essential to follow up with patients regularly, especially those at higher risk for prolapse. Screenings and open discussions about pelvic health can empower your patients to take charge of their well-being. Encourage them to voice their concerns and provide them with resources to manage or prevent symptoms effectively.
In conclusion, uterine and bladder prolapse might be common, but that doesn’t diminish its impact. As healthcare providers, we have a duty to listen, educate, and empower our patients. Engage in patient education and create a welcoming environment where women can feel comfortable discussing their health. This proactive approach not only fosters better health outcomes but also strengthens the bond between practitioners and their patients.
 Add Row
Add Row  Add
Add 




Write A Comment